Risk Of Postoperative Hemorrhage
Surgical intervention is associated with an increased risk of venous and arterial thromboembolism. It is also known that the temporary discontinuation of antithrombotic treatment leads to increased exposure to the risk of thrombosis and embolism.

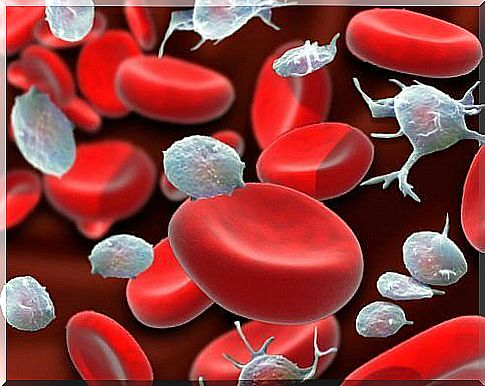
Postoperative bleeding problems can be the result of injury or trauma. They can also be explained by the way the blood clots. Different types of blood vessels carry oxygen and nutrients to the tissues. When the blood vessels or capillaries become damaged, bleeding can occur inside or outside.
Hemostasis is the stopping of bleeding from damaged blood vessels. The factors necessary for a clot to form are:
- Platelets : Platelets are very small cells produced by the bone marrow. The normal number of platelets is 150,000 to 400,000.
- Blood clotting factors: These factors are present in the blood and mainly occur in the liver.
Surgery is associated with an increased risk of venous and arterial thromboembolism. It is also known that the temporary interruption of antithrombotic treatment leads to an increased exposure to the risk of thrombosis and embolism.
The risk of preoperative bleeding from oral anticoagulants is generally low. However, it increases during and after surgery, depending on the nature of the surgery.
Risk factors for postoperative bleeding
An assessment of the risks associated with the surgery is necessary in this type of patient. For this reason, the type of action in relation to antithrombotic therapy is determined by the patient’s situation.
The risk of thrombosis and the risk of bleeding from the surgical intervention must be assessed. The thrombotic risk of the surgical intervention is taken into account because of the relation with the increased risk of thrombosis when the anticoagulant / antiaggregant treatment is stopped.
In these cases, the anticoagulant treatment can be continued or interrupted. Taking heparin can also replace it, before resuming treatment with oral anticoagulants. This is mainly explained by the post-surgical immobility, but also by the prothrombotic effect of the surgery itself.
Postoperative bleeding
Major bleeding is defined as bleeding that requires transfusion of more than two units, a second operation, or that causes bleeding in the intracranial, intrathoracic or peritoneal cavity.
The attitude towards any bleeding complication will depend on the extent and location of the bleeding. It also depends on the level of anticoagulation. Major bleeding is also defined as bleeding that is life-threatening or fatal.
The likelihood of bleeding will also determine the resumption of postoperative antithrombotic therapy, as the onset of anticoagulation will differ if there is a high risk of bleeding. If anticoagulation is removed for more than a day, heparin should be considered.
Resumption of anticoagulant therapy after surgery
Resumption of anticoagulant therapy after surgery should not start until 2 to 3 days after surgery. However, this should always be done after consultation with the specialist.
The use of therapeutic doses begins after 48-72 hours and should not take place after continuous post-surgical bleeding.
In most patients treated with both warfarin and acenocoumarol, treatment can be resumed the night of the day of the procedure. This can be the case as long as there are no bleeding complications.
However, the therapeutic effect will not begin until 4-5 days after the start of anticoagulant therapy. One of the main goals of the anticoagulated patient is to regain his antithrombotic state as quickly as possible. Consideration should be given to adequate postoperative hemostasis and the risk of bleeding associated with surgery.
Usually, most postoperative bleeding will go away within 24 hours of surgery. However, this may not be the case, so anticoagulation should not start until hemostasis returns to normal.